Matters of the heart – Coronary Arterial Disease (Part II) : How it happens and how food and lifestyle can help
Notes: 1. Do go back frequently to the previous post for reference. 2. As always, this post uses basic science and technology to simplify anatomical and physiological complexities thru ‘models’.
The critical and vulnerable nature of the coronary artery: It should be clear that:
 1. The coronary is the first branch of the aorta but a lot smaller in size which directly takes heart’s systolic pressure and has to bend and branch profusely as it supplies blood to the heart wall (myocardium). (Actually, it emerges from the aorta as a pair of branches meant to serves the right-left halves of the heart. Note here also, how blood vessels have to branch profusely, to spatially distribute/collect, blood to/from tissues).
1. The coronary is the first branch of the aorta but a lot smaller in size which directly takes heart’s systolic pressure and has to bend and branch profusely as it supplies blood to the heart wall (myocardium). (Actually, it emerges from the aorta as a pair of branches meant to serves the right-left halves of the heart. Note here also, how blood vessels have to branch profusely, to spatially distribute/collect, blood to/from tissues).
 2. Because of the way it has to be, it is vulnerable to developing pressure drops and ‘deposits’ (ref the ‘comparison’ in the previous post) on its inner surface which will begin to disturb the flow of blood past it. If it grows, its ‘pressure drop’ will be significant increasing the blood pressure upstream of it (raised systolic bp, hypertension) and reducing the flow downstream. If the deposit gets rooted in the arterial inner wall, it won’t lend itself to being ‘dislodged’ easily. If the deposit becomes hard because of mineral involvement, the pressure drop will be persistent and significant. If such a deposit comes loose because of suddenly forceful blood flow, it can block one of the smaller branches (plaque rupture) which can be triggered by sudden or new type of physical activity and be fatal.
2. Because of the way it has to be, it is vulnerable to developing pressure drops and ‘deposits’ (ref the ‘comparison’ in the previous post) on its inner surface which will begin to disturb the flow of blood past it. If it grows, its ‘pressure drop’ will be significant increasing the blood pressure upstream of it (raised systolic bp, hypertension) and reducing the flow downstream. If the deposit gets rooted in the arterial inner wall, it won’t lend itself to being ‘dislodged’ easily. If the deposit becomes hard because of mineral involvement, the pressure drop will be persistent and significant. If such a deposit comes loose because of suddenly forceful blood flow, it can block one of the smaller branches (plaque rupture) which can be triggered by sudden or new type of physical activity and be fatal.
 3. Reduced blood flow will inevitably restrict oxygen and nutrient supply to the part of the heart wall serviced by it. In an extreme case, the part can slowly ‘die’ leading to formation of a dead patch of myocardium called an ‘infarct’ (Myocardial infarction). To the extent of such infarction, there is now ‘less of heart’ than before; it has partially atrophied. Note that such blockages are a ‘double whammy’; they load the heart and reduce its capacity to carry that load.
3. Reduced blood flow will inevitably restrict oxygen and nutrient supply to the part of the heart wall serviced by it. In an extreme case, the part can slowly ‘die’ leading to formation of a dead patch of myocardium called an ‘infarct’ (Myocardial infarction). To the extent of such infarction, there is now ‘less of heart’ than before; it has partially atrophied. Note that such blockages are a ‘double whammy’; they load the heart and reduce its capacity to carry that load.
Such atherosclerosis can be of several types; fatty atherosclerosis is just a common type. Similarly, it can occur anywhere but the coronary is the first ‘convenient’ site that can precipitate serious, externally measurable effects.
Coronary Arterial Disease (CAD): (Ref ‘Pump-driven flow of water in a pipe’ in the previous post to serve as ‘model’.)
CAD is number one killer worldwide. This term is used for the above-mentioned condition of the heart led by atherosclerosis. It eventually leads to myocardial infarction. Your physician will tell you how useful (or otherwise) the electrocardiogram (ECG) and the echo-cardiogram are in detecting how far atherosclerosis and myocardial infarction have advanced.
 Angina is the chest pain resulting from myocardial infarction. Heart attack is the acute and often radiating pain on the left side of the chest when the atherosclerosis and infarction have advanced. Early markers: (i) Quick tiring. (ii) Raised blood lipid profile, especially ldl cholesterol. (iii) BMI rising above 30. (iv) Difficulty breathing. (iv) Own history of fatty food consumption and exercise levels. (v) Stress levels. (vi) Age. (vii) Elevated blood pressure. See your doctor if you experience chest or upper body discomfort, palpitations, sweating, shortness of breath or unexplained nausea.
Angina is the chest pain resulting from myocardial infarction. Heart attack is the acute and often radiating pain on the left side of the chest when the atherosclerosis and infarction have advanced. Early markers: (i) Quick tiring. (ii) Raised blood lipid profile, especially ldl cholesterol. (iii) BMI rising above 30. (iv) Difficulty breathing. (iv) Own history of fatty food consumption and exercise levels. (v) Stress levels. (vi) Age. (vii) Elevated blood pressure. See your doctor if you experience chest or upper body discomfort, palpitations, sweating, shortness of breath or unexplained nausea.
 Angiography is the radiology-assisted determination of where and how advanced atherosclerosis is. Angioplasty is the surgical procedure that reduces the arterial blockage by a stent – a meshy insert that dilates the artery around the blockage and restores the blood flow. Coronary bypass graft is the literal bypassing of the blocked portion of the artery with a healthy artery harvested from your body (often, the leg) – similar to the road bypasses when a stretch of the road is unusable.
Angiography is the radiology-assisted determination of where and how advanced atherosclerosis is. Angioplasty is the surgical procedure that reduces the arterial blockage by a stent – a meshy insert that dilates the artery around the blockage and restores the blood flow. Coronary bypass graft is the literal bypassing of the blocked portion of the artery with a healthy artery harvested from your body (often, the leg) – similar to the road bypasses when a stretch of the road is unusable.
Heart transplant – rarely resorted to – is the replacement of the defunct heart with a relatively healthy heart harvested from a recently expired person. Of course, severing and then restoring the elaborate ‘plumbing’ around the heart is challenging and is not for the faint of the heart. Usually this happens in an accident or when a patient dies of a heart-independent cause leaving a functional, usable and transplantable heart.
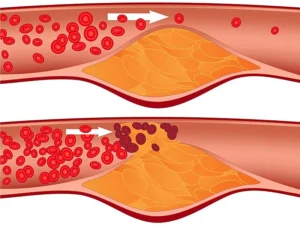 Plaque rupture and sudden death:If a person with a significant blockage suddenly starts vigorous or a new type of exercise, the deposit (also called plaque) can rupture because of the hastened blood flow thru an abnormal stumbling block in a compromised conduit. As we will see soon, the plaques are rooted in the arterial endothelium and this amounts to a ‘wound’ leading to a blood clot and plaque debris being released and carried by blood. This can block an artery branch and lead to instant death. The increasingly frequent reports of people collapsing and dying while performing garba or playing cricket or exercising or even on a stage at a public rally are often the result of plaque rupture. Note: This clearly indicates the importance of regular health/pathological check-ops and avoidance of adventurous sudden starts of unfamiliar exercise, especially in an excited state.
Plaque rupture and sudden death:If a person with a significant blockage suddenly starts vigorous or a new type of exercise, the deposit (also called plaque) can rupture because of the hastened blood flow thru an abnormal stumbling block in a compromised conduit. As we will see soon, the plaques are rooted in the arterial endothelium and this amounts to a ‘wound’ leading to a blood clot and plaque debris being released and carried by blood. This can block an artery branch and lead to instant death. The increasingly frequent reports of people collapsing and dying while performing garba or playing cricket or exercising or even on a stage at a public rally are often the result of plaque rupture. Note: This clearly indicates the importance of regular health/pathological check-ops and avoidance of adventurous sudden starts of unfamiliar exercise, especially in an excited state.
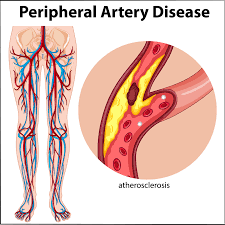
CAD, CHD, CVD, Cerebro-vascular Disease, PAD: CAD is the cluster of coronary conditions starting with partial blockage and the entire gamut of effects as it advances. CHD is the condition that adversely affects the heart – mostly but not exclusively, infarction. CVD is the cluster condition that follows the CAD-CHD combination and extends to the effects of blockage at all corners of the body. PAD – the Peripheral Arterial Disease, as the name suggests, is the atherosclerosis of the arteries on the periphery – mainly the lower limbs. Cerebro-vascular disease affects the blood supply to parts of the brain. In happening far from the heart, it resembles PAD. However, it can also stem from ‘cerebral embolism’ – a blood clot clogging one of its finer arteries – apart from fatty atherosclerosis. Its initial effect is difficulty in concentrating, slurred speech, drooping of one side of face, tottering…., the precipitate effect is a stroke causing paralysis.

How CAD develops – the factors approach: We will now call the deposits fatty plaques. Like all chronic conditions, CAD development seems to be caused by many factors: heredity, sedentary lifestyle, proneness to frequent and/or prolonged spells of negative feelings (anxiety, worry, anger, envy….), oil/fat rich diet, smoking, diabetes and obesity. However, this is not an exhaustive list and unexplained incidence is not uncommon. How these factors lead to plaque-promoting mechanisms is a complex issue beyond the scope of this blog.
How CAD develops – the mechanism: Surprisingly, the mechanism of initiation of the plaque formation (as the cumulative effect of factors) is not unanimously agreed but it is clear that plaques can start as early as teens as ‘streaks’ on the inside surface of the artery – the endothelium.
(A side note: We know that cholesterol and fat are not dissolved in the watery part of the blood; you have read several times on this blog how water and fat or cholesterol are totally different. Now, nothing really ‘belongs to’ blood if it is not soluble in water – its principal component. Salt, glucose and urea are soluble in water and will not separate out physically; their exit is with water. Physical separation of fats would be thermodynamically spontaneous. The curves and bifurcations in the coronary – the pressure drop origins – promote this spontaneity.
As an example, milk fat is colloidally (i.e. as fine droplets) dispersed in watery part of milk and cream separated from it is simply milk with fat content bumped up from 6-7% to 30-40%. This process is evocatively called ‘skimming’ in deference to the earliest skimming of cream from the top of settled milk. The ‘lean’ milk (containing < 1 % fat) then yields Skimmed Milk Powder (SMP) on drying. Home makers do it routinely to separate ‘malai’ from milk; smart ones do it on cold milk which has firm ‘malai’ that slides off easily.
Obviously, fat globules are packed more closely in cream than in milk and bringing them together is easy by ‘beating’ cream which increases energetic globule collisions. This encourages the fat globules to coalesce into a continuous mass with some trapped watery part and this is the newly formed butter. Your home-made butter contains less fat because of limits of domestic beating which incorporates a good amount of air and makes it light. You can cheat yourself into eating a large dollop of this fluffy white butter which provides limited fat! The remainder of the initial watery part is freed or released and settles below the large butter mass and is drained off. As you can see, fat dispersed in milk needed just some ‘encouragement’ to come together; it always wanted to happen; beating cream made it thermodynamically spontaneous.)
Some arterial endothelial damage seems to be the initiator of plaque formation. The flurry of events that follow is too complex but the essence is that a combination of ‘arterial wound’ and body’s inevitable immune response to it, fatty separation and a growing ‘hump’ are the initial plaque. Eventually, ldl – cholesterol, a non-water component of the plaque – is believed to get oxidized because of the presence of oxygen-rich molecules and free radicals in the blood and cause the ‘terminal’ reaction of an irreversible plaque lodged there. When the plaque gets mineralized and firmed up with calcium; the damage is done.
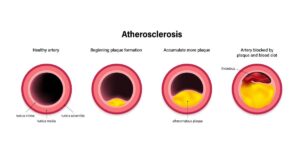 Source: Adobe Stock
Source: Adobe Stock
The aforesaid endothelial damage seems to be under-understood but let us logically treat frequent bouts of raised heart rate (rubbing the arterial endothelium hard) as the cause, inducing us to avoid them. A ramped up heart rate raises the blood pressure and typical triggers are: smoking, anxiety, anger, envy, worry, frustration, dissatisfaction….. The irony is that the BP rise caused by CAD is steady unlike the pre-atherosclerosis rises which are transient. The image of a self-sustaining scourge is complete. Note, however, that this ‘neat sequencing of causative events’ is a simplification
Note: the suppleness of arteries decreases with age because of the aging of smooth muscles embedded in them. We will see in the next post how this can contribute to rise in blood pressure. Obviously, be doubly careful as you age.
How food can help: Here’s a focused food advice on staving off CAD:
 Avoid hyperlipidemia i.e. excessive blood triglyceride and cholesterol (especially the ldl variety) by limiting calories contributed by oils/fats to less than 30 %, even less, if life is sedentary. Stay physically active (Ref posts on obesity) to ensure consumption of lipids for energy release rather than build up in the blood and migration to adipose tissue. Interestingly, triglycerides – logically candidates for separation out of blood – are not found in CAD plaques alluding that they tend to raise blood cholesterol levels rather than become part of the plaque themselves.
Avoid hyperlipidemia i.e. excessive blood triglyceride and cholesterol (especially the ldl variety) by limiting calories contributed by oils/fats to less than 30 %, even less, if life is sedentary. Stay physically active (Ref posts on obesity) to ensure consumption of lipids for energy release rather than build up in the blood and migration to adipose tissue. Interestingly, triglycerides – logically candidates for separation out of blood – are not found in CAD plaques alluding that they tend to raise blood cholesterol levels rather than become part of the plaque themselves.- PUFA oils not only provide essential fatty acids (ref post 19, The physiological roles of edible oils: They do a lot for us within our body) but also raise the good cholesterol (hdl) cholesterol and lower ldl-cholesterol. Let about 20 % of the oil/fat calories come from them. Use them smartly – we will soon devote an entire post on this very important aspect because they are prone to oxidation before they enter our body and be those oxygen-carriers that oxidize plaque ldl-cholesterol.
- Do not worry too much about saturated fatty acids if your bulk oils are not palm oil and coconut oil. Stearic acid, the most dominant natural sfa has now been exonerated of cholesterolemicity in moderate quantities. Avoid trans fats; the west has adequate regulatory measures in place and the rest needs to be cautious in consumption of hydrogenated fats.
 Adopt fruits and vegetables big time; they give you natural anti-oxidants to neutralize those oxygen carriers apart from providing dietary fiber and crowding out empty calories. Some day we will dive deep into novel ways of doing that; for now, adopt salads, pulpy juices, vegetable dishes, fruity yoghurts and soups. Innovate; we have a wonderful single-dish meal of a multiple daal-vegetables- green and dry spices dish. We often garnish our fruity platters with strawberry pulp. Our salads often contain both fruits and vegetables – typically with the aforesaid single-dish meal.
Adopt fruits and vegetables big time; they give you natural anti-oxidants to neutralize those oxygen carriers apart from providing dietary fiber and crowding out empty calories. Some day we will dive deep into novel ways of doing that; for now, adopt salads, pulpy juices, vegetable dishes, fruity yoghurts and soups. Innovate; we have a wonderful single-dish meal of a multiple daal-vegetables- green and dry spices dish. We often garnish our fruity platters with strawberry pulp. Our salads often contain both fruits and vegetables – typically with the aforesaid single-dish meal.
To supplement these measures,
 Stay physically active; don’t feel diffident because you don’t or can’t gym or formally exercise. You are the best judge of what works for you; brisk walking, manually washing clothes (as we do), cooking (as we delightedly do), manual dish washing, gardening, general household cleanup, climbing stairs, walking to the nearby market are good examples.
Stay physically active; don’t feel diffident because you don’t or can’t gym or formally exercise. You are the best judge of what works for you; brisk walking, manually washing clothes (as we do), cooking (as we delightedly do), manual dish washing, gardening, general household cleanup, climbing stairs, walking to the nearby market are good examples.- Stay positive. Relationships are good, so are social contacts and hobbies. It is important to go to bed satisfied and tired and rise fresh and excited. Life’s beautiful; don’t complicate it.
- Ask your physician for the best path analysis and its frequency for you; and learn to interpret it smartly – labs always tell you what ‘standards’ are and you can easily judge where you are above or below it. It is hugely empowering. When a cardiogram or echo-cardiogram or even angioplasty becomes necessary, embrace it. Even if you consider yourself young, healthy and symptom-free remember, that inevitable slippages in diet and exercise, bp-raising events, pollution, aging, heredity etc. can silently cause disturbances in the blood composition. These will come to the fore only thru pre-emptive testing. None of this is paranoia; information is power; keep it on your side. Combined with food-led help, you will find life exhilarating. We will talk about a great help in that direction some day.
4. Self help. Excellent digital blood pressure instruments are available economically; even physicians use them now. We routinely check our bp. Your physician will tell you what is best for you. With practice, you will learn to attribute a bp rise or depression on your own. Watch weight and track BMI.
Next Post:
Blood pressure and hypertension
Their nature, origin, effects and remedies with focus on food
Visit disclaimer
3 thoughts on “Matters of the heart – Coronary Arterial Disease (Part II) : How it happens and how food and lifestyle can help”
Wonderful paintings! That is the type of info that are meant to be shared around the web. Disgrace on the search engines for not positioning this publish higher! Come on over and seek advice from my web site . Thank you =)
Hello! Would you mind if I share your blog with my myspace group? There’s a lot of folks that I think would really enjoy your content. Please let me know. Thanks
Hi,
Thank you for the kind words. Feel free to share the blog with your myspace group.